May 12 2020
On May 8th, New England Journal of Medicine (NEJM) published letter to the editor by researchers from the Washington University School of Medicine, St. Louis titled “Collateral Effect of Covid-19 on Stroke Evaluation in the United States”.
Is this about “collateral damage” or strokes caused by SARS-CoV-2? It is not! Despite “talking heads” proclamations on national TV that the virus kills people left and right due to hyper-coagulation (increased clotting) with big and small emboli blocking blood supply to vital organs, the number of patients experiencing symptoms of stoke undergoing neuroimaging dropped 39% when comparing daily counts during “pre-pandemic” month of February of 2020 with 14-day period between March 26th through April 8th of 2020.
To make sure, the authors did not actually count stroke patients instead using a surrogate measure - the number of patients with ischemic stroke registered in a nationwide neuroimaging database. Neuroimaging (CT or MRI) is essential element of the “stroke protocol” used to direct care of patients experiencing stroke symptoms. Besides helping to diagnose stroke, it also determines who will benefit from endovascular thrombectomy - removal of clot occluding one of the major arteries supplying brain.
Thrombectomy is indicated in patients within 24-hour window of the time last known to be well. If successful, it may lead to complete alleviation of stroke consequences and full recovery. Hence, it is critical to seek medical care and undergo imaging sooner rather than later after onset of stroke symptoms.
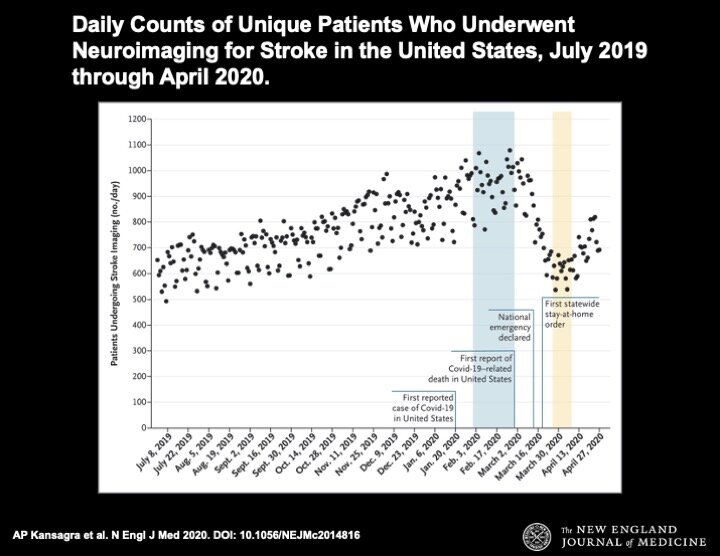
Authors analyzed data on 231,753 patients from 856 hospitals in the USA from July 1st, 2019 through April 27th, 2020. The results are presented in easy to understand graph reflecting daily counts.
Figure 1. Daily Counts of Unique Patients Who Underwent Neuroimaging for Stroke in the United States, July 2019 through April 2020.
All the neuroimaging tests were processed with RAPID software. Each dot represents a daily count of patients. Shaded regions correspond to the prepandemic (blue) and early-pandemic (yellow) epochs. The increase in the number of patients who underwent imaging from July 2019 to March 2020 reflects an increase in the number of hospitals that were using RAPID software.
The results surprised authors and everybody else. The number of daily cases increased from the low of 500 in early July of 2019 to the high of almost 1100 at the end of February of 2020 (this is explained by growing adoption of the software) and then … dropped back to just over 500 by the end of March of 2020. The decrease in the use of stroke imaging from the pre-pandemic epoch to the early-pandemic epoch was seen across all age, sex, and stroke severity subgroups, and occurred in most states regardless of the number of diagnosed COVID-19 cases.
Does this mean the number of patients with ischemic stroke dropped almost in half in one month? Did we find panacea for stroke prevention? Obviously not.
The only definitive conclusion, which can be made from this study, is that number of imaging evaluations in designated stoke centers dropped.
Does this mean that 40% less patients experienced stroke symptoms during pandemic? This lacks any plausible explanation.
Does this mean that SARS-CoV-2 prevents stroke?Let’s all get infected then!
Does this mean that number of patients experiencing stroke symptoms who seek care dropped 40%? This is hard to believe because:
How many of us would stay home while experiencing stroke? Only those who are unconscious and alone, or those who would rather die or get disabled by stroke than COVID-19. Dr. Why: It is kind of cool to be able to pick the way one dies!
How many family members seeing a loved one experiencing stroke symptoms would not call an ambulance? Only those who are ignorant or want patient to die…
How many ambulance crews would leave patient at home when stroke is suspected? None;
How many doctors who got a call from a patient or a family member would advise do nothing? None;
How many ER doctors at the designated stroke centers would not be familiar or unwilling to follow stroke protocol? None;
How many imaging departments will refuse to perform imaging for a suspected stroke? None;
How many hospitals were overwhelmed by COVID-19 patients nationwide and would not be able not accept stroke patients? Not many, even in NYC. It is a common knowledge that emergency departments nationwide experienced a sharp drop in volume and had to furlough medical staff, cut hours or salaries, or fire employees outright;
How many hospitals/or doctors would refuse to submit cases into the database? There is no incentive for non-reporting.
Got the point?
If not, here are the explanations which come to mind:
Stroke patients were misdiagnosed as … COVID-19;
Stroke patients were counted as … probable COVID-19;
Stroke patients were intentionally misclassified as … COVID-19.
Do you have a better explanation? I am eager to hear it.
P.S. The supplementary appendix to the letter contains more food for thought:
The reported cases included age groups from 0 to 85+ years old;
The states with the biggest drop in referrals include:
New Mexico - 232.9%
Wyoming - 75.6%
Indiana - 56.7%
Lousiana -51.2%
Colorado -50.3%
Washington - 50.2%
Maine - 49.3%
Michigan - 48.8%
Missouri - 47.9%
Arkansas - 47.6%
New York - 46%
Minnesotta - 44.1%
Maryland - 43%
California - 35.8%
The states with the smallest drop in referrals include:
South Dakota - 1.7%
New Jersey - 17.6%
Nevada - 19.6%
West Virginia - 20.1%
Oregon - 20.5%
The states where referrals increased include:
DC + 8.5%
Idaho + 7.5%
Arizona +4.1%